Current Neurosurgical Workflows
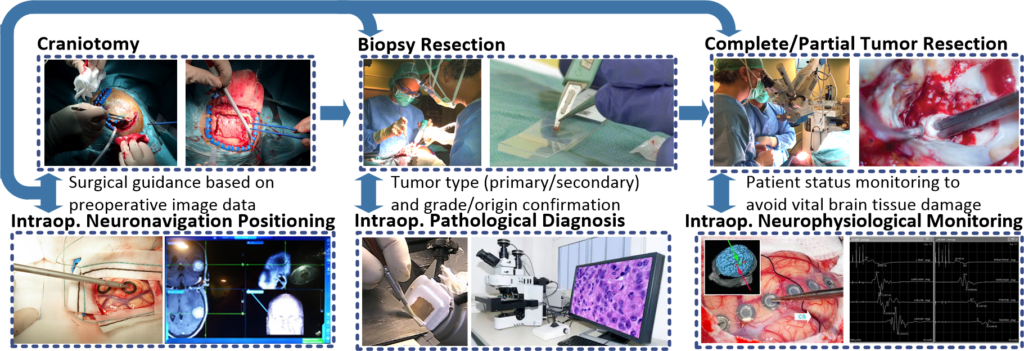
Neurosurgery is one of the main procedures carried out to treat brain tumours. In this treatment, the neurosurgeon makes an opening in the skull of the patient (called craniotomy) and, whenever possible, tries to resect the entire tumour tissue from the brain guided by a neurosurgical navigation system based on a preoperative image.
In neurosurgery, complete tumour resection significantly affects patient survival. In case the tumour cannot be fully resected without damaging vital brain tissue, the surgeon resects as much tumour as possible, reducing pressure on the brain and diminishing the amount of tumour to be treated by post-surgery radiation therapy or chemotherapy. Normally, during surgery a small piece of the tumour is resected and sent to an intraoperative pathological analysis where the pathologist examines the sample under a microscope to determine the types of cells (tumour type and grade or origin) it contains.
This intraoperative pathological diagnosis helps in the surgeon’s decision-making during tumour resection to apply the most suitable surgical treatment depending on the tumour type and grade. Moreover, other sources of information are employed to aid surgeons during the tumour resection, such as the intraoperative neurophysiological monitoring (IONM), to avoid vital brain tissue damages that can affect patient’s quality of life (QoL).
Neurosurgery challenges
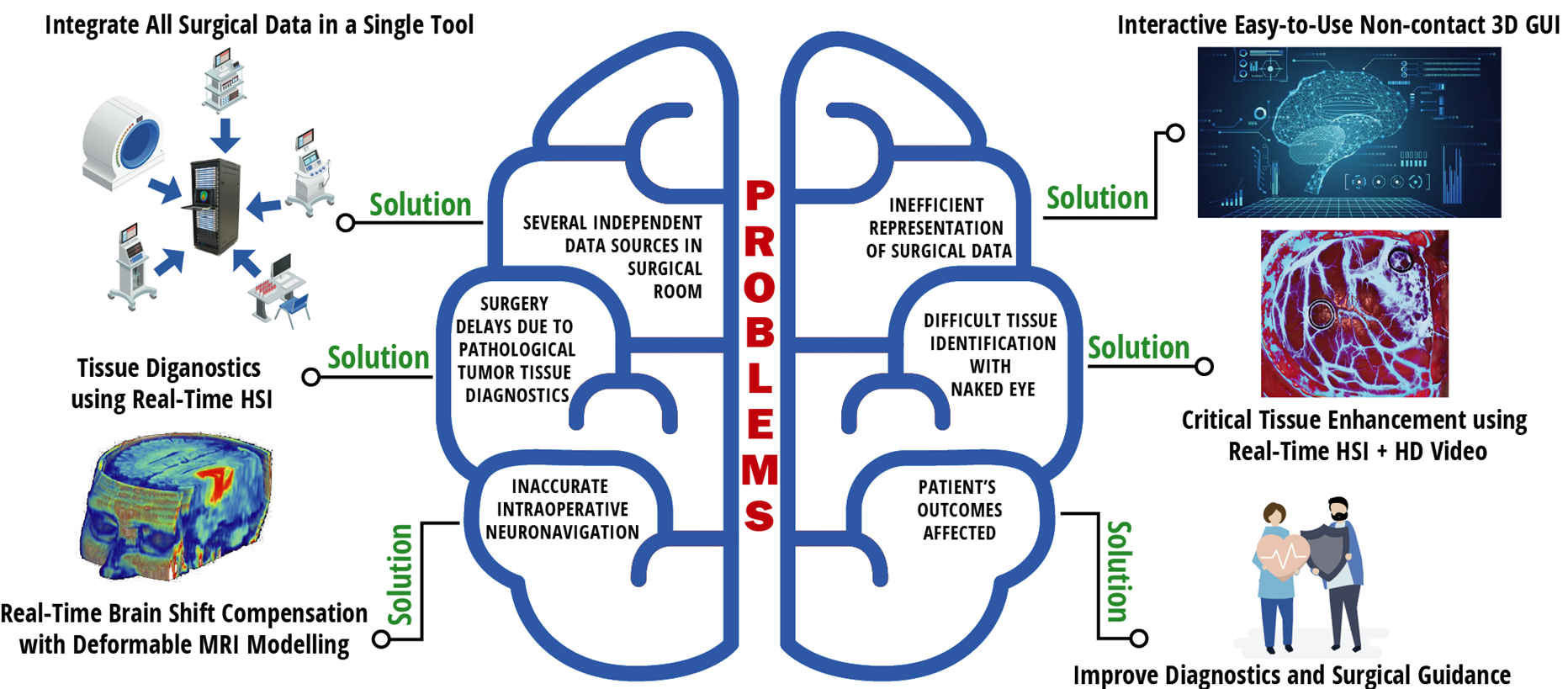
Neurosurgeons face the following challenges to address brain tumour surgeries trying to identify tumour mass and to differentiate among critical tissue or brain tumour margins during surgical procedures:
- Lack of specific tools to enhance the surgeons’ vision and to provide real-time personalized tissue diagnostics for surgical guidance and decision making.
- Lack of real-time representation, interpretation and analysis tools for big data acquired by various independent systems before and during the surgery.
- Long waiting times for intraoperative pathology consultation that can take up to 45 min, providing only a preliminary diagnosis of the tumour type by analysing a small piece of tissue resected.
- Non-existence of commercial tools for the analysis and visualisation of the brain shift phenomenon caused by the movement of the brain after performing the craniotomy and starting the resection.
- Potential side effects caused in the patient due to the use of photosensitive drugs or contrast agents because of employing specific fluorescent guidance tools.
A neurosurgical decision support tool able to provide quick, accurate and highly personalized diagnostics for optimal decision in neurosurgical practice will ensure a reduction of errors and delays during surgeries, and also save the medical costs associated to them.
Project Objectives
STRATUM will develop a 3D Decision Support Tool for brain surgery guidance and diagnostics (reaching TRL7) based on multimodal data processing using Artificial Intelligence (AI) algorithms, integrated as an energy-efficient Point-of-Care computing tool. The system will be developed following a co-creation methodology involving key stakeholders and end-users. STRATUM will pursue the following objectives:
SO-1
To foster advances in personalized medicine
SO-2
To increase the intraoperative diagnostic accuracy
SO-3
To reduce surgery time
SO-4
To improve cost- and energy-efficiency of surgery
SO-5
To clinically demonstrate the STRATUM prototype
SO-6
To prepare the business plan and the TRL9 roadmap
The STRATUM tool will exploit the interdisciplinary expertise of the 12 international partners in the Consortium, being developed following a co-creation methodology involving key stakeholders and end-users. The tool will integrate at least the following features:
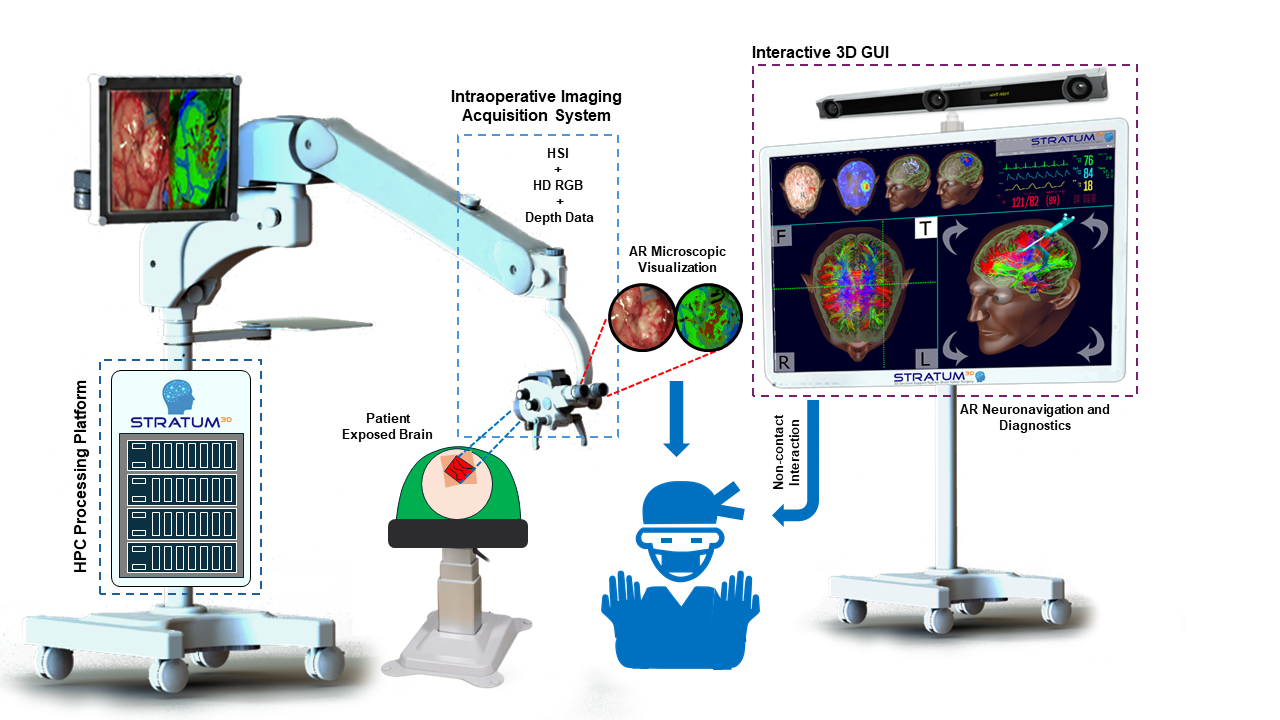
- Hyperspectral Imaging (HSI) system. HSI will be used as an image guidance and diagnostic mean. In addition, High-Definition video imaging and depth data will be also integrated in the tool, providing high spatial resolution information and depth information to generate 3D brain surface reconstructions that will offer accurate surgical guidance.
- Intraoperative Augmented Reality Neuronavigation based on pre-operative data, such as Magnetic Resonance Imaging (MRI) or Computed Tomography (CT), combined with HSI data. Brain shifts and deformations will be addressed in the loop to provide accurate intraoperative neuronavigation information. This will be shown to the surgeon via an interactive easy-to-use and non-contact 3D graphical user interface, where a 3D model of the patient’s brain combined with the diagnostic results of the algorithms will be shown to the surgeon.
- Intraoperative Neurophysiological Monitoring and life support systems. The integration of these data within the new tool will provide valuable feedback to neurosurgeons about the status of the surgery and the patient during the surgical procedure.
- High-Performance Computing platforms that will integrate, combine and interpret all the previously mentioned sources of data through innovative and robust AI algorithms, providing quick detailed, accurate and highly personalised diagnostics to drive brain surgeries in real-time.
Optimized integration and processing of available and new emerging data sources would help surgeons to make time-efficient and correct tissue removal decisions. This would maximize the degree of resection while minimising the risk of neurological deficits. Moreover, time-efficient surgical procedures not only benefit patients directly by minimizing anaesthesia time and risks such as postoperative infections, but also indirectly by optimizing healthcare resources.
Visit the project page on CORDIS, the European Commission’s primary public repository for EU-funded research projects.
Project Figures
- Name: 3D Decision Support Tool for Brain Tumor Surgery
- Acronym: STRATUM
- Grant Agreement ID: 101137416
- Start Date: 1 December 2023
- End Date: 30 November 2028
- Coordinator: University of Las Palmas de Gran Canaria (ULPGC)
- Consortium: 12 partners from 6 countries
- Total Cost: € 10,714,691.25
- EU Contribution: € 9,990,566.25